Abstract
The number of oncological patients who may benefit from proton beam radiotherapy (PBT) or carbon ion radiotherapy (CIRT), overall referred to as particle radiotherapy (RT), is expected to strongly increase in the next future, as well as the number of cardiological patients requiring cardiac implantable electronic devices (CIEDs). The management of patients with a CIED requiring particle RT deserves peculiar attention compared to those undergoing conventional photon beam RT, mostly due to the potential generation of secondary neutrons by particle beams interactions. Current consensus documents recommend managing these patients as being at intermediate/high risk of RT-induced device malfunctioning regardless of the dose on the CIED and the beam delivery method used, despite the last one significantly affects secondary neutrons generation (very limited neutrons production with active scanning as opposed to the passive scattering technique). The key issues for the current review were expressed in four questions according to the Population, Intervention, Control, Outcome criteria. Three in vitro and five in vivo studies were included. Based on the available data, PBT and CIRT with active scanning have a limited potential to interfere with CIED that has only emerged from in vitro study so far, while a significant potential for neutron-related, not severe, CIED malfunctions (resets) was consistently reported in both clinical and in vitro studies with passive scattering.
Similar content being viewed by others
Introduction
As a result of aging and comorbidities, the incidence of cancer and the use of cardiac implantable electronic devices (CIEDs) have increased concomitantly [1, 2]. A large Danish population-based cohort study including patients undergoing conventional photon beam RT reported that the annual rate of RT courses in pacemaker (PM)/implantable cardioverter–defibrillator (ICD) patients in Western Denmark was 4.33 per 100 000 person-years in 2012, representing an increment of 199% since 2003 [3].
As previously reported [4, 5], RT can induce CIEDs malfunctions as a result of several factors, including (1) stochastic effects associated with secondary neutrons interactions; (2) transient noise oversensing due to the RT dose rate used, with dose rates < 0.01 Gy/min considered at low risk; (3) the total cumulative dose delivered to the device's generator, with doses below 2 Gray (Gy) considered at low risk. Secondary neutrons can be produced, according to the RT type, energy and delivery method, by the nuclear interactions with the material in the beam path during treatment. These factors can lead to three types of CIED malfunctions: (1) Transient malfunctions, occurring only during RT exposure because of electromagnetic interferences; (2) Reverting to back-up setting (reset), a condition that can be either recovered after CIED programming or spontaneously resolve; (3) Permanent malfunctions, demanding CIED replacement. From a functional point of view, CIED malfunctions can be classified into hard errors due to damage to the hardware and most often related to direct irradiation and soft errors, due to software (random access memory) alterations and usually associated with scattered radiation or electromagnetic interference, being the reset a typical example of the latter group [6, 7]. Notably, except for a single case report in which a shock coil failure secondary to external irradiation was reported [8], there is no solid evidence in the literature suggesting a significant potential for a negative effect of RT on the electrodes in CIED systems. On the contrary, dedicated reports confirming the safety of RT on ICD leads despite high RT dosages (> 50 Gy) exist [9]. Currently, there is no safe threshold dose for the electrodes, the leads and the coils that are generally considered to be insensitive to radiation.
Proton beam therapy (PBT) and carbon ion RT (CIRT) have recently emerged as encouraging RT methods to limit radiation toxicity associated with conventional RT with photons while maintaining high rates of tumor local control for several malignancies [10,11,12,13]. Heavy ions such as protons and carbon ions have physical and biological advantages over photons: the so-called inverse dose deposition of particle beams allows the deposition of the majority of the energy at the end of their path in tissue, with limited dose in the entrance channel and beyond the target [11]. Moreover, their higher relative biological effectiveness (RBE) compared to photons allows delivering low physical dose to obtain the required therapeutic dose to the target. Notably, despite the limited available studies, in current consensus documents [13,14,15,16] patients with an implanted CIED and receiving PBT were considered at intermediate/high risk of RT-induced device malfunctioning, independently on the beam delivery method, on the estimated dose on the generator and on the generator and the tumor site. This assumption was based on the expected larger amount of secondary neutrons production by PBT as compared to conventional RT with energies below 10 MeV. Except for the recent European consensus document [16] that assigns to CIRT a low potential for RT-induced device mulfunctioning without providing any reference, no specific recommendations were provided for patients receiving CIRT, although there was a general warning to consider at high-risk patients receiving RT with a high potential for secondary neutrons production. The German guidelines express concerns about the delivery of PBT in patients with CIEDs without suggesting practical management strategies [17]. Finally, the recently released Polish expert opinion and consensus paper about cancer patients with CIEDs undergoing RT does not even address the issue of PBT and CIRT [18]. Of note, the amount of secondary neutron production induced by both PBT and CIRT is critically influenced by the beam delivery method, namely active scanning modality (also referred to as pencil beam scanning or spot scanning, in which a beam of particles is magnetically scanned across the field) rather than passive scattering (in which the beam is spread out laterally as a uniform beam through single or double scattering). The former is associated with very limited secondary neutron production [19, 20]. Nonetheless, 2017 American Guidelines recommend (Class I, level of evidence B not randomized) to prefer non-neutron-producing treatment over neutron-producing treatment in patients with a CIED to minimize the risk of device reset, therefore potentially depriving CIED patients of a life-saving treatment from an oncological point of view due to the presence of a CIED. On the contrary, patients receiving conventional RT are generally considered at high risk only in case of high dosages to the generator, of high energy photons, of PM dependency of the patient combined to the usage of high-energy photons, or of the presence of an ICD, particularly in case of a positive history for previous appropriate interventions. A recent paper shares the same approach [21]. Notably, for patients considered at high risk, intensive intra treatment monitoring and consideration for CIED relocation are recommended [13,14,15, 17, 18, 22].
Starting from these premises, the present work aims to review the literature data about CIEDs malfunction associated with PBT and CIRT and to provide an overview of the studies investigating the management of patients with CIEDs undergoing PBT or CIRT.
Material and methods
Search strategy
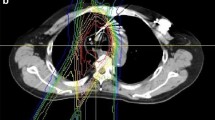
The key issue was expressed in four questions according to the Population, Intervention, Control, Outcome (PICO) design approach [23, 24]. These queries (Table 1) have been the matter of a literature search in the PubMed, Web of Science, and Scopus databases from 2000 to 2021 according to a combination of the following keywords: "Defibrillator," “Implantable Cardiac Device,” “Pacemaker,” “Radiotherapy,” “Hadrontherapy,” “Particle,” “Carbon Ions,” “Heavy Ions,” “Protons” including pluralization and US English/UK English spelling variations and suffixes/prefixes. We conducted a systematic search using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) literature selection process (Fig. 1) [25]. Two authors independently searched reference lists of recognized manuscripts to integrate the literature search.
Selection criteria for full-text article review
Papers were suitable for insertion in the review if the following criteria were fulfilled: (1) published as a full article in peer-reviewed journals; (2) PBT and CIRT techniques; (3) in vivo and/or in vitro study, (4) at least one of the considered outcomes (type of malfunction/management of malfunction/relationship with planning) reported; (5) articles written in the English language. Interventional, observational, prospective and retrospective studies were considered. Exclusion criteria were: (1) RT with other RT modalities than PBT or CIRT (brachytherapy, intraoperative RT, photon beam RT, electron beam RT); (2) single case reports, book chapters, books, or Conference Proceedings. A total of 8 publications met the inclusion and exclusion criteria, for a total of 3 in vitro studies and 5 in vivo studies.
Risk of bias
For each selected study, two investigators independently assessed the risk of bias to ensure validity and overcome eventual selection, performance, detection, attrition and reporting bias, according to Cochrane Handbook for Systematic Reviews of Interventions [26,27,28]. Bias across studies as well as bias and risks related to the source of funding and conflict of interest of authors of the included studies was assessed. Eventual disagreements were resolved through discussion.
Data collection
The data extraction form was validated by two researchers, and data were independently extracted by the two researchers.
Statistical analysis
Continuous variables are presented as mean ± standard deviation or as median (interquartile range [IQR]), while categorical variables are reported using counts and percentages. To compare variables, the Student’s t–test or the Mann-Whitney U test for continuous variables and the Chi-square or the Fischer exact test for categorical variables are used. A p value <0.05 was considered statistically significant.
Results
The selection of studies analyzed in the present review is shown in Fig. 1. Tables 2 and 3 show the studies characteristics; Supplemental Table 1 reports the risk of bias appraisal; Table 4 synthesizes the outcomes of the selected clinical studies.
Population
In vivo studies
Five retrospective [29,30,31,32,33] cohort studies published between 2008 and 2021 were included. A total of 157 patients (age range between 43 and 97 years old) who underwent 161 courses or particle-beam RT were included in the studies. Overall, 53 patients (34%) received thoracic RT for a thoracic tumor, 73 patients (46%) suffered abdominal or pelvis tumor, 27 patients (17%) had head-and-neck and skull base tumors, and 4 patients (3%) suffered bone and soft tissue sarcoma.
Finally, 135 patients (86%) had a PM and 22 (14%) an ICD. 15/81 (18.5%) patients with this information available were pacing-dependent. Except for one study that did not provide these data [33], dose constraints to the CIED’s power generator were maintained within the manufacturer and guidelines recommended limits by all the other studies (maximum dose of 2 Gy (RBE) or less) and the CIED was never located within the treatment field. Hashimoto et al. [33] did not provide information concerning CIED checking and intrasession monitoring; in contrast, in the remaining studies, each CIED was checked in advance before the first session. The two largest studies with available data (n = 73 patients, 83%) adopted intrasession monitoring with an in-room video system [30, 32]; in the remaining two studies with this information available, a continuous electrocardiography (ECG) monitoring was applied during each treatment fraction. In two studies [31, 32] (total 38 patients, 43%), the CIED was checked after each session, in one study weekly (n = 8, 9%)[29], in the last study (n = 42, 48%) [30] at the beginning and the end of RT.
In vitro studies
Three experimental studies were included [34,35,36] whose characteristics are reported below:
-
1.
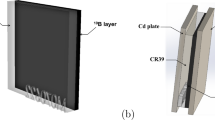
Hashimoto et al. [34] reported an experimental set-up study that simulated PBT delivered by passive scattering technique to ICD carriers. Four ICDs were placed in the phantom (0.3 cm laterally and 3 cm distally) outside the RT field of 10 × 10 cm2 with a total dose in-field of 107 Gy over 10 sessions of irradiation.
-
2.
Wootton et al. [35] investigated the proton dose perturbation due to a high-voltage coil on leads from ICDs in a water phantom reporting effects up to 20–35% as predicted by the treatment planning system (TPS) or measured using radiographic films.
-
3.
Bjerre et al. [36] evaluated the risk of malfunctions of pencil beam PBT in 49 CIEDs (50% PMs and 50% ICDs) located at a different distance from the Bragg’s Peak and the risk of noise, pace inhibition, and inappropriate shock therapy in 13 devices (9 ICDs, 69%) with connected leads that were monitored live during consecutive irradiations.
Intervention
In vivo studies
Most patients underwent PBT (124 patients, 79%), the remaining CIRT (32 patients, 20%), and one patient (1%) both. The total delivered dose ranged between 10 Gy(RBE) and 88 Gy(RBE).
In vitro studies
All studies [34,35,36] were performed with PBT.
Comparison
No randomized clinical trials (RCT) are available.
Outcomes
In vivo studies
None of the studies assessed the actual dose absorbed by the CIED. The distance between the RT field and the CIED generator ranged between 0 and > 50 cm. Two studies provide the distances between the CIED and the Planning Target Volume (PTV), in the range between 0.8 cm and 40 cm [30, 32]. In one study only, RT was preceded by phantom simulation that used the same CIED as those of the patients involved; that kind of simulation was able to predict 50% of reset cases [1 over 2]. The predictive value and the details of phantom stimulations are not reported for the 5 patients who did not develop CIED malfunctions in the same study. Only two studies reported the estimated maximum dose to the CIED of both protons and neutrons [30, 34]. Gomez et al. [30] calculated the neutron dose equivalent as a function of proton energy, aperture distance, field size, and width of the spread-out Bragg peak. Among the 42 patients of the study, the median estimated maximum proton and neutron doses to the CIED in all patients were 0.80 Gy(RBE) [range 0.13–2.1 Gy(RBE)] and 3.46 Sv (range 0.11–11 Sv). Among the three studies including ICD patients, only one (n = 31) [32] reported details about ICD programming management: asynchronous pacing stimulation or deactivation of anti-tachycardia treatments of ICD’s through reprogramming or magnet placement was not performed. Overall, 22 malfunctions were reported in 16/157 patients (overall incidence 10% of patients). The most frequently observed CIED malfunction was the reset to safety backup mode (17 cases in 13/157 patients, incidence 8% of patients), followed by 3 episodes of ICD oversensing (all in the same patient), one elective replacement indicator (ERI) and one enhanced impedance of the device lead which fluctuated. Notably, both the ERI status and the instability in the CIED lead impedance had already been detected before RT, with no additional unexpected changes occurring after RT. Therefore, the association with RT appears very unlikely. Only 2/10 of the reset cases with this information available were detected through the ECG, the remaining cases through CIED post-treatment check. All the 13 patients who had device resets were treated by passive scattering. None of the patients with CIED reset was pacing dependent; there was no need for urgent interventions, nor any patients developed symptoms. Overall, 7/10 cases (70%) of CIED reset with this information available were managed by CIED reprogramming; the remaining were transient and resolved either spontaneously ( = 1) [31] or after re-initialization of the CIED ( = 2) [29]. The patient with ERI status underwent uneventful elective generator replacement [30]; no further details were provided by Hashimoto et al. [33] concerning the patient who experienced 3 episodes of ICD oversensing, except for the fact that no permanent device malfunctions were observed.
Limited sub-analyses were performed according to the radiation site (thoracic vs not thoracic), the type of device (PM vs ICD), the type of beam scattering, the type of particle (passive scattering PBT vs CIRT) and the field to generation distance. For the purpose of this analysis, the cases of ERI and of lead impedance fluctuation, both unlikely to be related to RT because already existent before RT start, were not considered. The incidence of malfunctions (total n = 14 patients) was 0/41 (0%) among patients receiving active scanning beams as opposed to 14/116 (12%) among patients receiving passive scattering therapy (p for comparison = 0.02). Passive scattering PBT was not associated with a significantly higher rate of malfunctions as compared to passive scattering CIRT (14/104, 14% vs. 0/23, 0%, p for comparison = 0.07). No significant differences were found either according to the type of device: 10/135 (7%) in PM recipients versus 4/22 (18%) in ICD recipients (p for comparison = 0.111). Incidence of malfunction according to the site of RT was 8/53 (15%) for patients receiving thoracic RT as opposed to 6/104 (6%) for patients receiving not thoracic RT (p for comparison = 0.07). Punctual data concerning the field to generator distance within each patient were only available for 3 proton studies (n = 18 patients, all treated with passive scattering). The mean field to generator distance was 13.3 ± 11.6 cm in patients with CIED reset (n = 8) as opposed to 22.1 ± 14.3 in patients with no device malfunctions (p for comparison = 0.196). Hashimoto et al. [33] reported the distance between the edge of the irradiation field and the CIED only for the 20 patients with thoracic tumors: the incidence of malfunctions was 0/12 (0%) among patients with a distance between 0 and 15 cm, as compared to 2/8 (25%) among those with a distance > 15 cm (range 15–25, p for comparison = 0.147). In the study of Gomez et al. [30], among the 4 cases of reset, the mean maximum proton and neutron doses to the CIED generator were 0.745 Gy(RBE) and 655 mSv, respectively. Malfunctions happened at different cumulative delivered doses, ranging from 4 Gy(RBE) to 67.5 Gy(RBE) near the end of the PBT. Except for one study where this information was not available [33], all the other 10 cases of CIED resets took place at neutron doses to the device of at least 300 mSv.
In vitro studies
In the study of Hashimoto et al. [34], no permanent malfunctions were observed using passive scattering PBT. Overall, 29 soft errors occurred over 40 sessions (incidence 73% per session) with a rate of 1 soft error per 15 Gy and a rate of power-on resets (changes to safety back-up mode) of 1 per 50 Gy. The calculated dose of secondary scattered neutrons per 1 Gy was 1.3–8.9 mSv/Gy.
Wootton et al. [35] showed a significant potential for perturbation in the delivered PBT when the ICD high voltage lead was not moving, while movements miming the cardiorespiratory ones consistently reduced (albeit not eliminated) the potential for perturbation.
Finally, Bjerre et al. [36] described 61 reset errors (60 in Biotronik and 1 in Boston Scientific devices, none in Medtronic and St. Jude Medical devices) over 1728 fractions of active scanning PBT, with an overall incidence of reset of 4.9%, 2.8% and 1.6% per fraction at a lateral distance of 0.5, 5.0 and 10.0 cm, respectively. The risk was higher for each group for Biotronik device carriers (19.4%, 5.1%, and 3.2%, respectively). The risk was constant throughout the sessions, and, except for the 0.5 cm group, higher for ICDs than PMs. While all the resets that occurred in Biotronik devices were reprogrammed to normal function, the single error that occurred in the Boston Scientific device was permanent (the device was locked in permanent safety mode). Secondary neutron dose significantly augmented the odds of CIED resets by 55% per mSv. Battery depletion was observed in 5 devices (all Medtronic ICDs), albeit several conditions may have disrupted the calculations in these explanted evices. Finally, no cases of noise, over- or undersensing, pace inhibition or inappropriate shock therapy occurred during 362 fractions of live monitoring.
When comparing passive scattering PBT [33] with active scanning PBT [35] at a similar lateral distance (0.3 and 0.5 cm, respectively), the incidence of malfunctioning (all soft errors except for one) per session was significantly higher with passive scattering PBT (29/40, 73% vs. 42/864, 4.9%, p < 0.00001). The overall incidence of mulfunctionings with a lateral distance within 0.5 cm was 7.9% (71/904).
Discussion
To the best of our knowledge, our review represents the first study specifically addressing the topic of CIEDs malfunction associated with PBT and CIRT and including both in vivo and in vitro data. Concerning the key questions analyzed in the current review, according to PICO criteria, it emerges that:
-
Query 1: In vitro data are scant and only two studies [34, 36] were found using PBT and showing an important soft error potential with passing scattering PBT, and a significantly lower, but still not trivial, particularly for Biotronik devices, soft error potential with active scanning PBT. Notably, in the study using active scanning, no cases of intrasession noise, over- or undersensing, pace inhibition or inappropriate shock therapy occurred. A potential for battery depletion was reported for active scanning PBT, albeit this needs to be confirmed in vivo since several in vitro factors may have contributed. The last in vitro study [35] showed a potential for a mild perturbation of a moving high-voltage lead on the delivered proton beam.
-
Query 2: a total of 22 episodes of CIED malfunctions were observed in 16/157 patients undergoing 161 RT courses (overall incidence 10% of patients, 9% of RT courses), including 20 cases of CIED reset in 13 patients (incidence 8% of patients), 3 episodes of ICD oversensing (all in the same patient), one ERI condition and one increased (albeit fluctuating) lead impedance. The last two malfunctions were both pre-existing conditions before the beginning of RT sessions, and they were excluded from the sub-analyses on potential factors associated with CIED malfunctions. Therefore, no PBT/CIRT-related permanent malfunctions were observed (only resets or transient oversensing).
-
Query 3: no patients developed clinical symptoms during the reset episodes, which were mostly detected through ICD checks. Only one study provided information about the year of CIED implantation, while only the largest one [33] provided full details about the type of PM/ICDs for the patients with malfunctions and the presence/absence of a left ventricle lead.
-
Query 4: none of the 41 patients treated with active scanning developed CIED malfunctions, as opposed to 12% of patients receiving passive scattering therapy. A trend toward a higher incidence of CIED malfunctions was also experienced in thoracic vs not thoracic particle therapy as well as in passive scattering PBT versus passive scattering CIRT. No differences were observed according to the type of device (PM versus ICD).
The analyzed studies feature several limitations. Except for the multicentric study of Hashimoto et al. [33], the remaining studies represent single-center experiences, often with limited sample size. Moreover, patients and treatments were heterogeneous, and most studies lack details concerning the year of CIED implantation, the type of PM/ICDs and the number of leads (single-chamber versus dual-chamber versus cardiac resynchronization devices with a left ventricle lead). The latter might potentially influence both the incidence of hard errors due to lead damages as well as the patient’s symptoms during reset.
In the clinical studies, no differences were observed according to the type of device (PM versus ICD), but these findings might have been influenced by the inclusion of the latest ICD types, which were shown to be less sensitive to secondary neutrons scattering than the older ones [37]. Yet, the in vitro study [36] suggests a higher risk of ICDs than PMs. Concerning the type of device, an extensive review [38] predominantly including RT studies with photons and electrons (with only two PBT studies) showed that CIED malfunctions occur approximately in 3% of RT courses (with electrical reset being the most common ones). In the largest clinical study included in the review (560 CIED patients, 73 with ICD, photon RT only), Zaremba et al. [3] report a trend toward an increased risk of malfunctions in ICDs (6.8%) compared with PMs (2.5%). Subsequently, Aslian et al. [39] reported 6.9% of CIED malfunctioning during stereotactic RT. These data are in line with previous clinical reports [40]. Notably, in the large study by Zaremba [38], the location of the tumor was a strong predictor of CIED malfunction at univariable analysis, but its effect consistently declined after adjustment for beam energy [38]. This result supports the concept that soft errors such as electrical resets are mostly related to beam energy and secondary neutron scattering independently from the direct exposure to ionizing radiation. Secondary neutrons have been previously measured by various detectors [19] or estimated by Monte Carlo simulation [20, 41] using phantoms that are designed to represent human tissue. As already mentioned, the rate of neutron production in particle RT strongly depends on the dose delivery modality, and passive scattering yields much higher rates of out-of-field scattered neutrons, whereas active scanning allows for a significant dose advantage in neutron productions. This advantage has been estimated as a factor of at least 10 [42] and potentially even more (between 30 and 45) [43]. An Italian group recently reported the first in man case of active scanning PBT (single dose of 25 Gy-RBE), for the treatment of refractory ventricular tachycardia in a non-oncological PM-dependent patient with a biventricular ICD. No malfunctions were observed despite intensive intrafraction and post-therapy monitoring [44]. Yet, it has to be acknowledged that, as opposed to the very good safety profile emerged so far from the limited clinical experience of active scanning PBT [30, 32], pre-clinical studies mandate caution for the risk of reset (particularly for Biotronik devices) and the potential for battery depletion, while being extremely reassuring on the zero risk of more severe types of intrafraction malfunctionings such as pace inhibition or inappropriate shock therapy. Notably, there were only 4 patients with Biotronik devices in the clinical study by Seidensaal et al. [32].
PBT, based on the expected higher number of secondary scattered neutrons produced by protons as compared to photons with energies below 10 MeV, is considered at intermediate/high risk of CIED malfunction by all the consensus documents written so far [13,14,15, 17], while the management of patients receiving RT with CIRT is not specifically addressed. When comparing carbon ions with protons, several factors must be considered. On one side, neutron rate production with CIRT is expected to be higher due to nuclear fragmentation [45]. On the other side, the lower scattering both in air and in tissues of carbon ions, compared to protons, should lead to a reduction in the low dose region surrounding the target where presumably the device can be found. For these types of ion species, same for helium or oxygen, for instance, further investigations both in terms of real patient treatments and Monte Carlo simulation are needed.
Practical implications and discrepancies among consensus documents
From a practical standpoint, patients considered at high risk of RT-induced CIED malfunctions require a closer level of monitoring. The 2017 HRS expert consensus statement [14] recommends performing a continuous visual and voice contact during each RT fraction in all CIED patients receiving RT, but a strong recommendation for a weekly complete CIED evaluation was made only for patients undergoing neutron-producing treatment. For the other patients, a complete CIED evaluation was recommended after the end of the course of RT. No specific recommendations were provided concerning the eventual need for and the timing of ECG monitoring or intrasession pulse monitoring. On the other side, according to the 2019 AAPM TG-203 report [15], CIED patients receiving neutron-producing RT should undergo ECG weekly monitoring, but there are no specific recommendations concerning intersession CIED monitoring. Finally, an Italian consensus document [13] recommends, for patients receiving PBT, intrasession ECG or pulse oximeter plus audiovisual monitoring, CIED in office or remote evaluation after the first session and then weekly. The same approach is shared by the recent European consensus document [16].
Based on the clinical studies included in the present review, 20% of the reset cases were detected through the ECG, the remaining cases through CIED post-treatment check. Notably, in the only study [29] where two reset cases were detected through the ECG, the CIEDs were checked weekly. On the contrary, in the other three studies with this information available [30,31,32] including the one published in 2019 [32] CIEDs were checked after each session; moreover, in the study by Gomez et al. [30], CIEDs were also re-programmed in advance (before each session) to detect a reset from the pulse rate.
Due to the high incidence of reset to safety backup mode in patients receiving passive scattering heavy-ions RT based on studies with intensive ICD checking, it would seem reasonable to implement the same kind of monitoring, including at least a CIED check after each session in all patients. A continuous intrasession ECG or pulse monitoring (in addition to the visual and voice contact) could be limited to pacing-dependent and ICD patients, particularly in case of previous ventricular arrhythmias. The management of patients receiving last generation, active scanning heavy-ions RT (both PBT and CIRT) is more controversial, due to the actual discrepancy between the limited clinical data, suggesting an almost zero risk of malfunctions, and in vitro data (based on PBT only) showing an overall low but not null potential for reset events, almost exclusively in Biotronik device carriers, and for battery depletion. Based on in vitro data, patients with a Biotronik devices, those with an ICD and those pacing dependent should probably be checked after each session, while the other patients could receive weekly complete in person CIED evaluations combined to remote CIED monitoring to collect safety data before and after each session.
Conclusions
The available clinical and preclinical data consistently suggest a significant potential for neutron-related, not severe, electrical CIED malfunctions (asymptomatic resets) in patients receiving passive scattering particle RT. Accordingly, all these patients should be managed as a high-risk category until additional predictors or modulators of CIED malfunction risk are identified. On the contrary, clinical data on patients receiving the last generation, active scanning particle RT, albeit limited, disclose a promising safety profile, with no cases of CIED malfunctions reported so far. Yet, in vitro data still mandate caution for the risk of reset and potentially of battery depletion related to active scanning particle RT. Overall, the management of CIED patients receiving particle therapy is still extremely heterogeneous across centers. The safety profile of particle RT for CIED carriers may change in the next future due to technological improvements in both CIEDs and particle therapy, that is seeing the ongoing construction of several new centers worldwide. Still, it emerges an urgent call for shared protocols, as well as minimum criteria for scientific reporting.
References
Zhan C, Baine WB, Sedrakyan A, Steiner C (2008) Cardiac device implantation in the United States from 1997 through 2004: a population-based analysis. J Gen Intern Med 23(Suppl 1):13–19. https://doi.org/10.1007/s11606-007-0392-0
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424. https://doi.org/10.3322/caac.21492
Zaremba T, Jakobsen AR, Søgaard M, Thøgersen AM, Johansen MB, Madsen LB, Riahi S (2015) Risk of device malfunction in cancer patients with implantable cardiac device undergoing radiotherapy: a population-based cohort study. Pacing Clin Electrophysiol 38:343–356. https://doi.org/10.1111/pace.12572
Riva G, Alessandro O, Spoto R, Ferrari A, Garibaldi C, Cattani F, Luraschi R, Rondi E, Colombo N, Giovenzana FLF et al (2018) Radiotherapy in patients with cardiac implantable electronic devices: clinical and dosimetric aspects. Med Oncol 35:73. https://doi.org/10.1007/s12032-018-1126-3
Souliman SK, Christie J (1994) Pacemaker failure induced by radiotherapy. Pacing Clin Electrophysiol 17:270–273. https://doi.org/10.1111/j.1540-8159.1994.tb01387.x
Hashii H, Hashimoto T, Okawa A, Shida K, Isobe T, Hanmura M, Nishimura T, Aonuma K, Sakae T, Sakurai H (2013) Comparison of the effects of high-energy photon beam irradiation (10 and 18 MV) on 2 types of implantable cardioverter-defibrillators. Int J Radiat Oncol Biol Phys 85:840–845. https://doi.org/10.1016/j.ijrobp.2012.05.043
Langer M, Orlandi E, Carrara M, Previtali P, Haeusler EA (2012) Management of patients with implantable cardioverter defibrillator needing radiation therapy for cancer. Br J Anaesth 108:881–882. https://doi.org/10.1093/bja/aes113
John J, Kaye GC (2004) Shock coil failure secondary to external irradiation in a patient with implantable cardioverter defibrillator. Pacing Clin Electrophysiol 27:690–691. https://doi.org/10.1111/j.1540-8159.2004.00513.x
Lee JW, Seol KH (2019) Inevitable high-dose irradiation to lead of implantable cardioverter defibrillator in small cell lung cancer: a case report. J Med Case Rep 13:187. https://doi.org/10.1186/s13256-019-2111-y
Durante M, Loeffler JS (2010) Charged particles in radiation oncology. Nat Rev Clin Oncol 7:37–43. https://doi.org/10.1038/nrclinonc.2009.183
Tinganelli W, Durante M (2020) Carbon ion radiobiology. Cancers 12(10):3022. https://doi.org/10.3390/cancers12103022
Hwang EJ, Gorayski P, Le H, Hanna GG, Kenny L, Penniment M, Buck J, Thwaites D, Ahern V (2020) Particle therapy toxicity outcomes: a systematic review. J Med Imaging Radiat Oncol 64:725–737. https://doi.org/10.1111/1754-9485.13036
Zecchin M, Severgnini M, Fiorentino A, Malavasi VL, Menegotti L, Alongi F, Catanzariti D, Jereczek-Fossa BA, Stasi M, Russi E et al (2018) Management of patients with cardiac implantable electronic devices (CIED) undergoing radiotherapy: a consensus document from Associazione Italiana Aritmologia e Cardiostimolazione (AIAC), Associazione Italiana Radioterapia Oncologica (AIRO). Associazione Int J Cardiol 255:175–183. https://doi.org/10.1016/j.ijcard.2017.12.061
Indik JH, Gimbel JR, Abe H, Alkmim-Teixeira R, Birgersdotter-Green U, Clarke GD, Dickfeld T-ML, Froelich JW, Grant J, Hayes DL et al (2017) HRS expert consensus statement on magnetic resonance imaging and radiation exposure in patients with cardiovascular implantable electronic devices. Hear Rhythm 2017(14):e97–e153. https://doi.org/10.1016/j.hrthm.2017.04.025
Miften M, Mihailidis D, Kry SF, Reft C, Esquivel C, Farr J, Followill D, Hurkmans C, Liu A, Gayou O et al (2019) Management of radiotherapy patients with implanted cardiac pacemakers and defibrillators: a report of the AAPM TG-203(†). Med Phys 46:e757–e788. https://doi.org/10.1002/mp.13838
Stühlinger M, Burri H, Vernooy K, Garcia R, Lenarczyk R, Sultan A, Brunner M, Sabbag A, Özcan EE, Ramos JT, Di Stolfo G (2022) EHRA consensus on prevention and management of interference due to medical procedures in patients with cardiac implantable electronic devices. EP Europace. https://doi.org/10.1093/europace/euac040
Gauter-Fleckenstein B, Israel CW, Dorenkamp M, Dunst J, Roser M, Schimpf R, Steil V, Schäfer J, Höller U, Wenz F (2015) DEGRO/DGK guideline for radiotherapy in patients with cardiac implantable electronic devices. Strahlenther Onkol 191:393–404. https://doi.org/10.1007/s00066-015-0817-3
Tajstra M, Blamek S, Niedziela JT, Gadula-Gacek E, Przybylski A, Blicharz J, Oręziak A, Miszczyk L, Gepner K, Fijuth J et al (2019) Patients with cardiac implantable electronic devices undergoing radiotherapy in Poland. Expert opinion of the heart rhythm section of the polish cardiac society and the polish society of radiation oncology. Kardiologia Polska 77(11):1106–1116. https://doi.org/10.33963/KP.15063
Yonai S, Matsufuji N, Kanai T, Matsui Y, Matsushita K, Yamashita H, Numano M, Sakae T, Terunuma T, Nishio T et al (2008) Measurement of neutron ambient dose equivalent in passive carbon-ion and proton radiotherapies. Med Phys 35:4782–4792. https://doi.org/10.1118/1.2989019
Yonai S, Matsufuji N, Kanai T (2009) Monte Carlo study on secondary neutrons in passive carbon-ion radiotherapy: identification of the main source and reduction in the secondary neutron dose. Med Phys 36:4830–4839. https://doi.org/10.1118/1.3220624
Fradley MG, Lefebvre B, Carver J, Cheung JW, Feigenberg SJ, Lampert R, Liu J, Rajagopalan B, Lenihan DJ (2021) How to manage patients with cardiac implantable electronic devices undergoing radiation therapy. JACC CardioOncol 3:447–451. https://doi.org/10.1016/j.jaccao.2021.08.005
Escande A, Frey P, Lacornerie T, Mervoyer E, Chargari C, Laurans M, Mornex F, Marijon É, Giraud P (2022) Radiotherapy for patient with cardiac implantable electronic device, consensus from French radiation oncology society. Cancer Radiother J la Soc Fr Radiother Oncol 26:404–410. https://doi.org/10.1016/j.canrad.2021.11.003
Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S (2014) PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res 14:579. https://doi.org/10.1186/s12913-014-0579-0
Aslam S, Emmanuel P (2010) Formulating a researchable question: a critical step for facilitating good clinical research. Indian J Sex Transm Dis AIDS 31:47–50. https://doi.org/10.4103/0253-7184.69003
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012. https://doi.org/10.1016/j.jclinepi.2009.06.005
Boutron I, Page M, Higgins J, Altman D, Lundh A, Hróbjartsson A. “Considering bias and conflicts of interest among the included studies,” in Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021), ed. Cochrane, Chapter 7. Available at: Available from www.training.cochrane.org/handbook
Schünemann H, Higgins J, Vist G, Glasziou P, Akl E, Skoetz N, Guyatt G. “Completing ‘Summary of findings’ tables and grading the certainty of the evidencele,” in Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021) ed. Cochrane, Chapter 14. Available at: Available from www.training.cochrane.org/handbook
Higgins J, Altman D, Sterne J. “Assessing risk of bias in included studies,” in Higgins JPT, Churchill R, Chandler J, Cumpston MS (editors), Cochrane Handbook for Systematic Reviews of Interventions version 5.2.0 (updated June 2017), ed. Cochrane, Chapter 8. Available at: Available from www.training.cochrane.org/handbook
Oshiro Y, Sugahara S, Noma M, Sato M, Sakakibara Y, Sakae T, Hayashi Y, Nakayama H, Tsuboi K, Fukumitsu N et al (2008) Proton beam therapy interference with implanted cardiac pacemakers. Int J Radiat Oncol Biol Phys 72:723–727. https://doi.org/10.1016/j.ijrobp.2008.01.062
Gomez DR, Poenisch F, Pinnix CC, Sheu T, Chang JY, Memon N, Mohan R, Rozner MA, Dougherty AH (2013) Malfunctions of implantable cardiac devices in patients receiving proton beam therapy: incidence and predictors. Int J Radiat Oncol Biol Phys 87:570–575. https://doi.org/10.1016/j.ijrobp.2013.07.010
Ueyama T, Arimura T, Ogino T, Kondo N, Higashi R, Nakamura F, Ito S, Yoshiura T, Hishikawa Y (2016) Pacemaker malfunction associated with proton beam therapy: a report of two cases and review of literature—does field-to-generator distance matter? Oxford Med Case Rep 2016(8):omw049. https://doi.org/10.1093/omcr/omw049
Seidensaal K, Harrabi SB, Scholz E, Ellerbrock M, Haberer T, Weykamp F, Mattke M, Welte SE, Herfarth K et al (2019) Active-scanned protons and carbon ions in cancer treatment of patients with cardiac implantable electronic devices: experience of a single institution. Front Oncol. https://doi.org/10.3389/fonc.2019.00798
Hashimoto T, Demizu Y, Numajiri H, Isobe T, Fukuda S, Wakatsuki M, Yamashita H, Murayama S, Takamatsu S, Katoh H et al (2021) Particle therapy using protons or carbon ions for cancer patients with cardiac implantable electronic devices (CIED): a retrospective multi-institutional study. Jpn J Radiol. https://doi.org/10.1007/s11604-021-01218-1
Hashimoto T, Isobe T, Hashii H, Kumada H, Tada H, Okumura T, Tsuboi K, Sakae T, Aonuma K, Sakurai H (2012) Influence of secondary neutrons induced by proton radiotherapy for cancer patients with implantable cardioverter defibrillators. Radiat Oncol 7:10. https://doi.org/10.1186/1748-717X-7-10
Wootton LS, Polf JC, Peterson S, Wilkinson J, Rozner MA, Balter PA, Beddar S (2012) Proton dose perturbations caused by high-voltage leads from implanted cardioverter defibrillators. J Appl Clin Med Phys 13:3813. https://doi.org/10.1120/jacmp.v13i4.3813
Bjerre HL, Kronborg MB, Nielsen JC, Høyer M, Jensen MF, Zaremba T, Lægdsmand PMT, Søndergaard CS, Nyström H, Kronborg CJS (2021) Risk of cardiac implantable electronic device malfunctioning during pencil beam proton scanning in an in vitro setting. Int J Radiat Oncol Biol Phys 111:186–195. https://doi.org/10.1016/j.ijrobp.2021.03.053
Zecchin M, Morea G, Severgnini M, Sergi E, Baratto Roldan A, Bianco E, Magnani S, De Luca A, Zorzin Fantasia A, Salvatore L et al (2016) Malfunction of cardiac devices after radiotherapy without direct exposure to ionizing radiation: mechanisms and experimental data. Europace 18:288–293. https://doi.org/10.1093/europace/euv250
Zaremba T, Jakobsen AR, Søgaard M, Thøgersen AM, Riahi S (2016) Radiotherapy in patients with pacemakers and implantable cardioverter defibrillators: a literature review. Europace 18:479–491. https://doi.org/10.1093/europace/euv135
Aslian H, Kron T, Longo F, Rad R, Severgnini M (2019) A review and analysis of stereotactic body radiotherapy and radiosurgery of patients with cardiac implantable electronic devices. Australas Phys Eng Sci Med 42:415–425. https://doi.org/10.1007/s13246-019-00751-8
Solan AN, Solan MJ, Bednarz G, Goodkin MB (2004) Treatment of patients with cardiac pacemakers and implantable cardioverter-defibrillators during radiotherapy. Int J Radiat Oncol Biol Phys 59:897–904. https://doi.org/10.1016/j.ijrobp.2004.02.038
Morávek Z, Bogner L (2009) Analysis of the physical interactions of therapeutic proton beams in water with the use of Geant4 Monte Carlo calculations. Z Med Phys 19:174–181. https://doi.org/10.1016/j.zemedi.2009.04.006
Schneider U, Agosteo S, Pedroni E, Besserer J (2002) Secondary neutron dose during proton therapy using spot scanning. Int J Radiat Oncol Biol Phys 53:244–251. https://doi.org/10.1016/s0360-3016(01)02826-7
Clasie B, Wroe A, Kooy H, Depauw N, Flanz J, Paganetti H, Rosenfeld A (2010) Assessment of out-of-field absorbed dose and equivalent dose in proton fields. Med Phys 37:311–321. https://doi.org/10.1118/1.3271390
Dusi V, Vitolo V, Frigerio L, Totaro R, Valentini A, Barcellini A, Mirandola A, Perego GB, Coccia M, Greco A et al (2020) First-in-man case of non-invasive proton radiotherapy for the treatment of refractory ventricular tachycardia in advanced heart failure. Eur J Heart Fail. https://doi.org/10.1002/ejhf.2056
Weber U, Kraft G (2009) Comparison of carbon ions versus protons. Cancer J 15:325–332. https://doi.org/10.1097/PPO.0b013e3181b01935
Funding
Open access funding provided by Università degli Studi di Torino within the CRUI-CARE Agreement. The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare no conflict of interest.
Human and animal rights
The present review does not include human participants and/or animals; therefore, no informed consent was needed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Amelia Barcellini and Veronica Dusi share the first authorship.
Roberto Rordorf and Ester Orlandi share the last authorship.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Barcellini, A., Dusi, V., Mirandola, A. et al. The impact of particle radiotherapy on the functioning of cardiac implantable electronic devices: a systematic review of in vitro and in vivo studies according to PICO criteria. Radiol med 127, 1046–1058 (2022). https://doi.org/10.1007/s11547-022-01520-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-022-01520-6